Routine ultrasound-guided percutaneous transluminal angioplasty (PTA) is a feasible treatment for native arteriovenous fistula (AVF) dysfunction, according to a recent study by Antonio Granata (“Cannizzaro” Hospital, Catania, Italy). The findings were published online on 25 July in the Journal of Vascular Access (JVA).
Routine ultrasound-guided percutaneous transluminal angioplasty (PTA) is a feasible treatment for native arteriovenous fistula (AVF) dysfunction, according to a recent study by Antonio Granata (“Cannizzaro” Hospital, Catania, Italy). The findings were published online on 25 July in the Journal of Vascular Access (JVA).
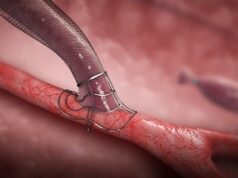
Granata et al note that stenosis is the main cause of arteriovenous fistula (AVF) failure and is due to neointimal hyperplasia. They describe PTA as the gold standard for patients with vascular access stenosis and aimed to evaluate the efficacy and safety of ultrasound-guided PTA in the treatment of native AVF venous stenosis.
The investigators determined the need for intervention by physical examination and duplex ultrasound in 162 patients. All patients with failing or not maturing AVF were treated in the outpatient setting under ultrasound guidance.
Granata and colleagues evaluated procedural success with repeated post-procedural ultrasound examinations. All procedures were performed under local anaesthesia by a single nephrologist and were performed in a single vascular laboratory, while follow-up ultrasound was performed in the dialysis unit of destination.
Writing in JVA, the authors detail that early technical success was obtained in 95.6% of cases (154 of 162) and complications occurred in 22 patients (13.5%) with no major complication requiring surgical or fluoroscopic endovascular intervention.
In addition, they noted that primary patency at six and 12 months was 84% and 69.8%, respectively. Risk factors for AVF failure/secondary PTA were vascular access low blood flow rate and vintage, as well as the need for thrombolysis during the first PTA.
Speaking to Vascular News, the authors commented that the method is particularly indicated in patients who still have residual diuresis.