This article forms part of an educational supplement sponsored by Shockwave Medical. Explore the full Shockwave L6 series here.

Charting the history of treatment for severely calcified iliac arteries, Michel Bosiers (University Hospital Bern, Bern, Switzerland) explains how the Shockwave L6—which is now available in selected EU markets—could change the game.
Large-vessel calcification, particularly in the iliac arteries, poses a significant challenge in vascular interventions. Severely calcified lesions increase the risk of major complications, such as vessel rupture, dissection, and distal embolisation during endovascular treatment. The current approach to managing iliac calcification primarily relies on established techniques like balloon angioplasty and stenting, whether using covered or noncovered stents.
In the past, the debate focused on whether to use self-expandable stents or balloonexpandable stents,1 with a preference for self-expandable stents. However, the advantage of self-expandable stents in calcified lesions seems to have diminished, likely due to the higher radial outward force of balloon-expandable stents. The COBEST trial (not sponsored by Shockwave Medical) compared the use of covered balloonexpandable stents versus bare-metal stents (BMS) and demonstrated the benefit of using covered balloon-expandable stents in treating TASC C and D lesions, outperforming BMS.2 Covered stents, with their polytetrafluoroethylene (PTFE) coating, are not only designed to protect against rupture, but can also mitigate against neointimal proliferation compared to BMS.3
A recently published systematic review confirmed the efficacy of covered stents over BMS in treating TASC C and D lesions. The primary patency rate for covered stents was 91.4% at 48 months, compared with 83.4% in the BMS group.4
 However, these methods have notable limitations, including the risks mentioned earlier and the potential for under-expansion of deployed stents in heavily calcified lesions. Under-expansion can lead to early failure due to in-stent restenosis or occlusion. While stenting has shown better patency rates compared to standard balloon angioplasty, many randomised controlled trials are underpowered or consist of single-arm studies, with calcification often under-evaluated. Consequently, the optimal treatment approach for severe iliac calcification remains unclear, highlighting the need for improved methods or alternative strategies.
However, these methods have notable limitations, including the risks mentioned earlier and the potential for under-expansion of deployed stents in heavily calcified lesions. Under-expansion can lead to early failure due to in-stent restenosis or occlusion. While stenting has shown better patency rates compared to standard balloon angioplasty, many randomised controlled trials are underpowered or consist of single-arm studies, with calcification often under-evaluated. Consequently, the optimal treatment approach for severe iliac calcification remains unclear, highlighting the need for improved methods or alternative strategies.
Although stenting offers proven benefits, successful outcomes require meticulous vessel preparation to ensure procedural safety. In many cases, the complexity of iliac calcification demands careful pre-stenting strategies to minimise complications, or the use of covered stents to mitigate the risk of rupture during excessive dilation in calcified lesions. This raises an important question: can stenting be entirely avoided through better preparation techniques or alternative approaches?
In recent years, Shockwave introduced its peripheral intravascular lithotripsy (IVL) system, designed for lithotripsy-enhanced, low-pressure balloon dilatation of calcified, stenotic peripheral arteries. The system includes a generator, connector cable, and an IVL catheter equipped with an array of lithotripsy emitters enclosed within an integrated balloon. A cohort analysis from the Disrupt PAD III observational study—a prospective, non-randomised, multicentre, single-arm study evaluating the real-world safety and effectiveness of the Shockwave peripheral IVL system for treating de novo calcified lesions in peripheral arteries—was published in 2020, focusing on its use in the iliac arteries. In total, 118 patients were treated using a 6 or 7mm IVL catheter (larger sizes were not yet available), with a stent placed in 72.9% of cases. No flow-limiting dissections, ruptures, or distal embolisations were observed, supporting the safety of this technology.5 However, it is not uncommon to encounter larger iliac arteries, and IVL therapy is most effective when the balloon is oversized by approximately 10% over the reference vessel diameter.
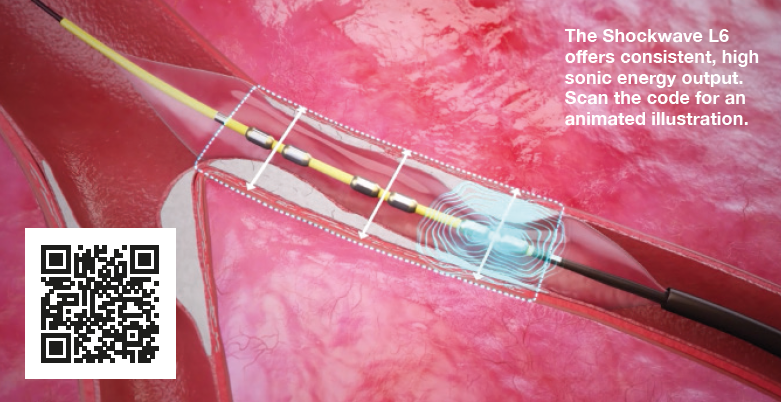
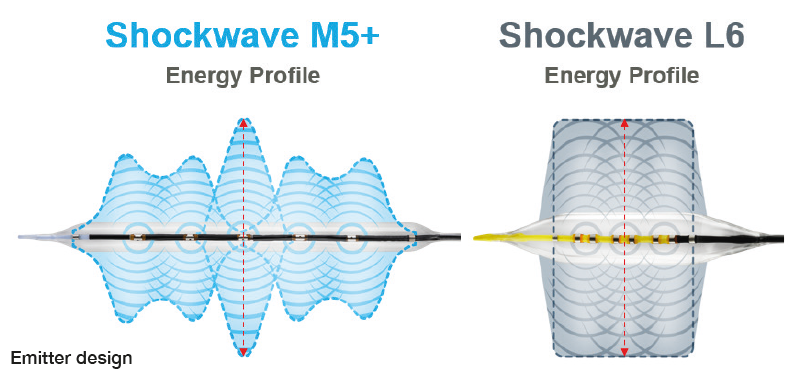 In this context, the introduction of the Shockwave L6 catheter offers a promising advancement. The Shockwave L6 is designed to overcome the limitations of current practices with its advanced features. The device offers a range of sizes from 8 to 12mm, which is crucial for treating larger iliac vessels, particularly given the need for 10% oversizing with IVL technology to maximise energy transfer into the vessel wall. This 1:1.1 ratio has already been proven safe in numerous trials. Additionally, Shockwave L6 IVL requires ultra-low delivery pressures of 2–4atm, further enhancing the safety and reducing the risk of dissection and rupture in a high-risk vascular bed. The compact emitter design of the Shockwave L6, with six emitters condensed into a 30mm integrated balloon length, creates uniform high energy across its entire length, providing efficient remodelling in challenging common iliac artery and external iliac artery cases with no compromise on safety. Moreover, the use of a 0.018” guidewire provides extra support compared to the 0.014” wire currently used with the M5 and M5+, which is particularly beneficial in larger and sometimes tortuous vessels. The amalgamation of these new features suggests a significant shift in how iliac calcification can be managed, potentially reducing the need for stenting and improving procedural outcomes.
In this context, the introduction of the Shockwave L6 catheter offers a promising advancement. The Shockwave L6 is designed to overcome the limitations of current practices with its advanced features. The device offers a range of sizes from 8 to 12mm, which is crucial for treating larger iliac vessels, particularly given the need for 10% oversizing with IVL technology to maximise energy transfer into the vessel wall. This 1:1.1 ratio has already been proven safe in numerous trials. Additionally, Shockwave L6 IVL requires ultra-low delivery pressures of 2–4atm, further enhancing the safety and reducing the risk of dissection and rupture in a high-risk vascular bed. The compact emitter design of the Shockwave L6, with six emitters condensed into a 30mm integrated balloon length, creates uniform high energy across its entire length, providing efficient remodelling in challenging common iliac artery and external iliac artery cases with no compromise on safety. Moreover, the use of a 0.018” guidewire provides extra support compared to the 0.014” wire currently used with the M5 and M5+, which is particularly beneficial in larger and sometimes tortuous vessels. The amalgamation of these new features suggests a significant shift in how iliac calcification can be managed, potentially reducing the need for stenting and improving procedural outcomes.
The Shockwave L6 has the potential to revolutionise the management of severe iliac calcification, offering a paradigm shift that may preserve treatment options while enhancing patient safety.5 The cases that follow will illustrate how the Shockwave L6 device could change current practices, address existing limitations, and set a new standard for managing large vessel calcification in the iliac arteries.
References
- Krankenberg H, Zeller T, Ingwersen M, et al. Self-expanding versus balloon-expandable stents for iliac artery occlusive disease: The randomized ICE trial. JACC Cardiovasc Interv. 2017 Aug 28;10(16):1694–1704. doi: 10.1016/j. jcin.2017.05.015. PMID: 28838480.
- Mwipatayi BP, Sharma S, Daneshmand A, et al; COBEST coinvestigators. Durability of the balloon-expandable covered versus bare-metal stents in the Covered versus balloon expandable stent trial (COBEST) for the treatment of aortoiliac occlusive disease. J Vasc Surg. 2016 Jul;64(1):83–94.e1. doi: 10.1016/j.jvs.2016.02.064. Epub 2016 Apr 28. PMID: 27131926.B.
- Dolmatch B, Dong YH, Heeter Z. Evaluation of three polytetrafluoroethylene stent-grafts in a model of neointimal hyperplasia. J Vasc Interv Radiol. 2007 Apr;18(4):527–534.
- Bontinis V, Bontinis A, Giannopoulos A, et al. Editor’s Choice – Covered stents versus bare metal stents in the treatment of aorto-iliac disease: A systematic review and individual participant data meta-analysis. Eur J Vasc Endovasc Surg. 2024 Sep;68(3):348–358. doi: 10.1016/j.ejvs.2024.06.008. Epub 2024 Jun 12. PMID: 38876369.
- Armstrong EJ, Soukas PA, Shammas N, et al. Intravascular lithotripsy for treatment of calcified, stenotic iliac arteries: A cohort analysis from the Disrupt PAD III study. Cardiovasc Revasc Med. 2020 Oct;21(10):1262–1268. doi: 10.1016/j. carrev.2020.02.026. Epub 2020 Mar 2. PMID: 32147133.
Michel Bosiers is a senior consultant at University Hospital Bern in Bern, Switzerland. He is a paid consultant of Shockwave Medical and his views expressed are not necessarily those of Shockwave Medical.












