Lorenzo Patrone talks to Vascular News about retrograde access to lower limb arterial chronic total occlusions (CTOs).
What
The retrograde approach to lower limb arterial chronic total occlusions was originally described more than thirty years ago1–3 but is still sometimes considered taboo.
Who?
I strongly believe that every operator should master the retrograde approach to lower limb arterial CTOs. I routinely run workshops on advanced lower limb recanalisations at my institution, which are open to motivated vascular surgeons and interventional radiologists. The retrograde approach is one of my main focuses during the course, offering the possibility to learn tips and tricks from my recorded and live cases.
When?
The retrograde approach to CTOs should be used sooner rather than later during the procedure in order to increase the recanalisation success rate, thus avoiding having to reschedule the patient for another endovascular procedure/bypass.
I personally use the retrograde approach in 30–40% of my cases, when I struggle more than five to 10 minutes in re-entering into the distal true lumen or when I perforate the vessel during the recanalisation attempt from the antegrade access. The recanalisation success rate using this approach is extremely high. Furthermore, it allows you to preserve the distal landing zone of the occluded artery with the potential subintimal dissection just limited to the occluded arterial segment.
Where?
The distal superficial femoral artery, proximal anterior tibial artery, dorsalis pedis artery and posterior tibial artery are the preferable choices but any artery can potentially be punctured in a retrograde fashion, as described in literature over the last decade.4,5
Why?
The retrograde access has almost always been described as a bailout solution after failed standard antegrade approach. The recently published C-TOP classification6 has shown how the on-table morphology of the plaque can already predict if patients could benefit from a retrograde approach. This could then be used as the first approach to treating the CTO (a higher rate of successful intraluminal recanalisation from the retrograde approach is described in the literature when compared to the antegrade one7), or to increase the chances of final success by reconnecting with the antegrade wire in the middle of the occluded artery.
The retrograde access is almost always used to exteriorise the wire from the antegrade access. In very rare cases it can be used as the main or even only access from where to introduce balloons or stent.8
How?
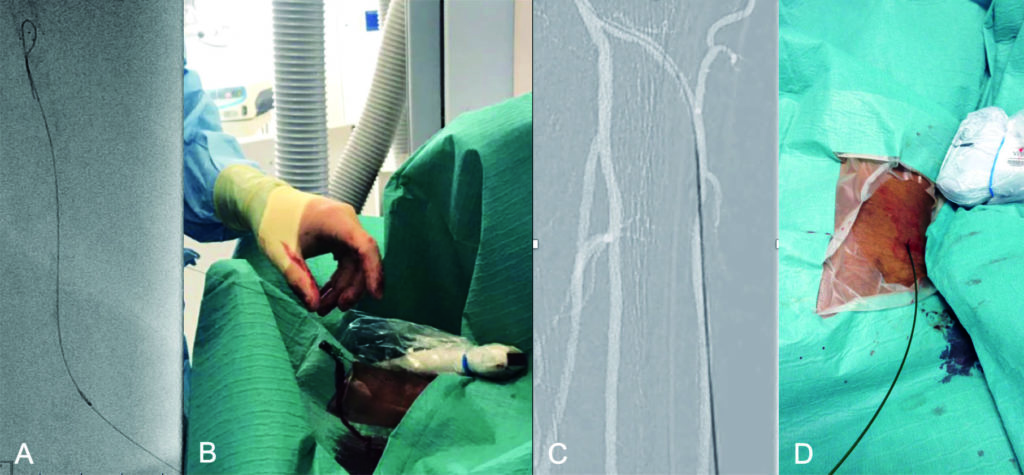
Retrograde access can be obtained by ultrasound or fluoroscopic guidance, depending on the skill set of the operator and the location/anatomy of the chosen artery. The distal SFA, dorsalis pedis artery and distal posterior tibial artery are usually easily accessible under ultrasound. This approach presents the advantages of better accuracy, real time visualisation of the needle (particularly important in case of patient under local anaesthesia), and avoids radiation exposure to the operator.
The fluoroscopic guidance is, on the other hand, easier to manage for any operator and preferable for retrograde access through a peroneal or proximal anterior tibial artery puncture. Proficient use of fluoroscopic filters can minimise the radiation exposure to the operator. In this method the needle needs to be advanced at 45 degrees to the skin while keeping it completely in line with the artery to minimise the chance of missing the artery.
The very vast majority of retrograde accesses do not require the insertion of a sheath, and an 0.018’’ wire and a compatible catheter are usually sufficient to cross the occlusion. The actual outer diameter of the sheath is always 2Fr bigger than the indicated size, so by going sheath-less one avoids greater trauma to the punctured vessel.
Angioplasty alone at the level of the retrograde access site is enough to obtain haemostasis in the majority of cases.
Ten tips and tricks
- The bigger the vessel, the easier the puncture. I think that the distal SFA is probably the most suitable target for someone who wants to start practising in retrograde punctures. If the operator feels comfortable with ultrasound, a good trick could be to scan the patient’s distal thigh by ultrasound before starting the operation and mark on the skin at the level of a possible entry point (remember, however, that if the same distal SFA will be punctured under fluoroscopic guidance the access site will significantly change, being more medial). To have a sterile window already prepared before starting with the recanalisation reduces the effort in getting the access at a later stage.
- When puncturing under fluoroscopic guidance, try to zoom in on your potential retrograde access site to increase your accuracy.
- The needle which I routinely use is the 21Gx7cm one which is part of any micropuncture kit. I then use a 21Gx15cm Chiba needle when the body habitus of the patient suggests to me that the distance to the distal superficial femoral artery, proximal anterior tibial artery, or peroneal artery is longer than in the majority of patients.
- Always use a 0.018”x300cm long wire, which has to be passed through the needle as soon as the puncture is made because you will benefit from all its length once the wire is through the antegrade and the retrograde access.
- There is never the need to position the patient prone for a distal SFA/popliteal access. A moderate extrarotation of the knee permits to reach the distal SFA and the proximal popliteal artery in the vast majority of the cases under ultrasound or fluoroscopic guidance. If needed, the tibioperoneal trunk and the distal popliteal artery can be punctured under fluoroscopic guidance through the interossea membrane.7
- Always remember that, when puncturing a deep vessel as the distal superficial femoral artery, the proximal anterior tibial artery, or the peroneal artery under fluoroscopic guidance, you will hit the vessel roughly 4–5cm above your skin entrance. I therefore suggest you to keep at least 7–8cm between your puncture site and the distal occluded vessel, in order to achieve sufficient stability once the wire needs to be inserted and the recanalisation starts.
- Always avoid surgical exposure of the vessels at the level of the ankle, especially in critical limb ischemia patients. The ultrasound approach for these vessels is usually relatively easy and the percutaneous access avoids possible difficult wound healing in already arterially compromised patients.
- There are different ways to externalise the wire advanced from the retrograde access. One is to try to pass it into a catheter advanced from the antegrade access (6F for the above-knee vessels and 4F for the below-knee ones); the other one is to use a snare, inserted from the antegrade access, to grab it. In my practice, I now approach all the long SFA occlusions with an initial over the hill common femoral artery access in order to facilitate grabbing a wire inserted through a retrograde approach by withdrawing my sheath/ catheter to the level of the external iliac artery.
- Another important trick, useful for patients who need to be punctured distally under fluoroscopic guidance and are not under general or spinal, is to avoid the local anaesthesia before the retrograde puncture. It will be easier and quicker to puncture the distal vessel without getting movement artefacts due to the stinging of the local anaesthesia which can then be easily provided once the retrograde access is secured by the insertion of the wire.
- Finally, when puncturing distal vessels under fluoroscopic guidance, remember to use one hand to advance the needle and the other one to simultaneously hold the foot. In case the patient moves between the angiogram and the puncture, you can always align the vessel to your reference image again with small controlled movements of the foot.
Lorenzo Patrone is a vascular and interventional radiology consultant at the West London Vascular and Interventional Centre (Northwick Park Hospital, London, UK).
References
- Tønnesen KH, Sager P, et al. Percutaneous transluminal angioplasty of the superficial femoral artery by retrograde catheterization via the popliteal artery. Cardiovasc Intervent Radiol 1988 Jun;11(3):127-31.
- Botti CF Jr, Ansel GM, et al. Percutaneous retrograde tibial access in limb salvage. J Endovasc Ther 2003 Jun;10(3):614-8
- Spinosa DJ, Leung DA, et al. Simultaneous antegrade and retrograde access for subintimal recanalization of peripheral arterial occlusion. J Vasc Interv Radiol. 2003 Nov;14(11):1449-54
- Palena LM, Manzi M. Extreme below-the-knee interventions: retrograde transmetatarsal or transplantar arch access for foot salvage in challenging cases of critical limb ischemia. J Endovasc Ther 2012 Dec;19(6):805-11.
- Silvestro M, Palena LM, et al. Anterolateral retrograde access to the distal popliteal artery and to the tibioperoneal trunk for recanalization of femoropopliteal chronic total occlusions. J Vasc Surg 2018 Dec;68(6):1824-1832.
- Saab F, Jaff MR, et al. Chronic Total Occlusion Crossing Approach Based on Plaque Cap Morphology: The CTOP Classification. J Endovasc Ther 2018 Jun;25(3):284-291.
- Fanelli F, Cannavale A. Retrograde recanalization of complex SFA lesions indications and techniques. J Cardiovasc Surg (Torino) 2014 Aug;55(4):465-71.
- Mustapha JA, Saab F, et al. Tibio-pedal arterial minimally invasive retrograde revascularization in patients with advanced peripheral vascular disease: the TAMI technique, original case series. Catheter Cardiovasc Interv 2014 May 1;83(6):987-94.