Shockwave Medical has announced positive clinical results from the pooled DISRUPT PAD Study, a single-arm, two-phase, multicentre study evaluating the safety and performance of the company’s Lithoplasty system in calcified peripheral lesions.
Results from 95 patients with symptomatic femoropopliteal lesions up to 15cm in length enrolled at 11 sites were presented at the VIVA 16 meeting in Las Vegas by principal investigator Thomas Zeller, head of the Department of Angiology at Universitäts-Herzzentrum Freiburg-Bad, Krozingen, Germany.
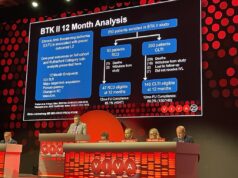
The DISRUPT PAD study primary safety endpoint was freedom from major adverse events through 30 days. Procedural success, the primary performance endpoint, was defined as less than 50% residual diameter stenosis, with or without adjunctive balloon angioplasty therapy. Key secondary endpoints include target lesion revascularisation, target lesion patency by duplex ultrasound defined as freedom from greater than 50% restenosis, and functional outcomes.
“The ongoing positive results from DISRUPT PAD demonstrate that Lithoplasty technology is a promising treatment for patients with calcified peripheral artery disease, a difficult-to-treat population,” says Zeller. “After six months of follow-up, we have documented consistent and predictable procedural success, high acute gain, minimal vessel injury, and remarkably low need for additional implants.”
Clinical data from the study demonstrate compelling safety with no major amputations, perforations, thrombus or distal embolisation events. Stent utilisation due to a flow limiting dissection following Lithoplasty was limited to 1% in study population composed of moderate or severely calcified lesions.
Primary effectiveness results demonstrated 100% procedural success defined as residual stenosis <50%. An exploratory endpoint of procedural success defined as residual stenosis <30% was achieved in 89.5% of lesions, with an average residual stenosis of 24% and acute gain of 3mm (average RVD of 5.5mm). Six-month patency assessed by duplex ultrasound was 77% with target lesion revascularisation of 3.2%.
Designed to overcome the limitations of currently available interventional devices Lithoplasty is a novel technology that uses pulsatile mechanical energy waves to disrupt both superficial and deep calcium while minimising soft tissue injury using an integrated balloon to dilate lesions at low pressures to restore blood flow.
The company plans to initiate a limited US commercial release in 2017, and plans to initiate a global randomised trial to gather further clinical data on the benefits of Lithoplasty treatment, according to a press release.