
Addressing representatives from the US Food and Drug Administration (FDA) and UK Medicines and Healthcare products Regulatory Agency (MHRA) directly, Thomas Zeller (Bad Krozingen, Germany) argued at the Charing Cross (CX) Digital Edition 2021 (19–22 April, online) that “it is time to change the agency recommendations regarding paclitaxel use in peripheral interventions”. Moderators Andrew Holden (Auckland, New Zealand) and Gunnar Tepe (Rosenhein, Germany), Podium 1st presenters Gary Ansel (Columbus, USA) and William Gray (Wynnewood, USA), as well as a 71% majority of the CX audience, supported this view. While there was agreement that it was right to be concerned about the paclitaxel mortality signal raised by Konstantinos Katsanos (Patras, Greece) et al in their December 2018 meta-analysis, there was strong consensus that the evidence is now clear there is no mortality effect when paclitaxel is used in the peripheral arteries. In addition, it was noted that several individual patient-level meta-analyses failed to confirm the high mortality signal flagged by Katsanos and colleagues. There was some discussion surrounding the place of limus as an alternative to paclitaxel, but experts agreed that there is no need to move to another drug—which would have its own set of challenges—given the proven safety and efficacy of paclitaxel. The takeaway message was clear: that, with proper caution and the correct dose, paclitaxel can and should be used in peripheral interventions.
All Peripheral Arterial Proximal sessions are available to view on demand. Click here to register and access the recordings.
More data find no mortality associated with paclitaxel
Patient safety has been at the centre of CX discussion on the paclitaxel issue since the Katsanos meta-analysis was published. This year, further data were presented that support the conclusion of vascular pathologist Elena Ladich (Hollywood, USA) who two years ago at CX 2019 stated that there are “no causal links or mechanisms to explain the reported association of paclitaxel in the lower limbs and patient mortality”.
Sabine Steiner (Leipzig, Germany) gave the first presentation on long-term paclitaxel data at CX 2021, outlining five-year results of the REAL-PTX study—an investigator-initiated, prospective, European, multicentre randomised controlled trial (RCT) comprising 150 patients with femoropopliteal disease. Patients were randomised to treatment with either a drug-eluting stent (100% Zilver PTX, Cook) or a drug-coated balloon (DCB; 77.3% IN.PACT Admiral/IN.PACT Pacific, Medtronic; 21.3% Lutonix, BD). Steiner reported that mortality rates after five years were “comparable to prior reports investigating long-term outcomes for drug-eluting and non-drug-eluting devices”.
Registrants can view this presentation on demand here.
Also presenting data in support of the safety of paclitaxel, Mårten Falkenberg (Gothenburg, Sweden) gave the latest analysis and interpretation of the SWEDEPAD trial concerning mortality. “It is very unlikely that devices coated with paclitaxel used for the treatment of peripheral arterial disease [PAD] do increase late mortality”, he concluded.
Registrants can view this presentation on demand here.
In a Podium 1st presentation on the topic, Andrew Holden (Auckland, New Zealand), on behalf of co-authors Ramon Varcoe (Sydney, Australia) and Peter Schneider (San Francisco, USA), revealed a five-year meta-analysis update regarding drug-coated technologies in femoropopliteal interventions and all-cause mortality concerns that included the SWEDEPAD update. Holden stressed that there is a “clear benefit of paclitaxel-coated devices in femoropopliteal disease” and relayed that the investigators recommend the continued use of these devices in this patient population. “The time has arrived for regulators to provide updated and clear guidance on these devices for the benefit of patients globally”, he stated.
Registrants can view this presentation on demand here.
Consensus that paclitaxel recommendations need to be changed
With a growing pool of data showing no association between paclitaxel and mortality, representatives from the FDA and MHRA reiterated current agency positions on the topic. Sara Royce, team lead of the plaque modification devices team at the FDA, talked the CX audience through regulatory approaches to the next-generation of drug-coated devices for PAD. Roopa Prabhakar, senior medical devices specialist at the MHRA, offered a UK perspective on paclitaxel device regulation, saying the agency will “continue to assess the significance of any new data in relation to patient safety”.
Registrants can view Royce’s presentation on demand here and Prabhakar’s presentation here.
Following these presentations, Thomas Zeller argued that it is time to change the agency recommendations regarding paclitaxel use in peripheral interventions. “Withholding such devices to patients with severe peripheral arterial occlusive disease may even harm them and result in increased global healthcare costs”, he stated, concluding that “the benefit outweighs the hypothetical risk”.
Registrants can view this presentation on demand here.
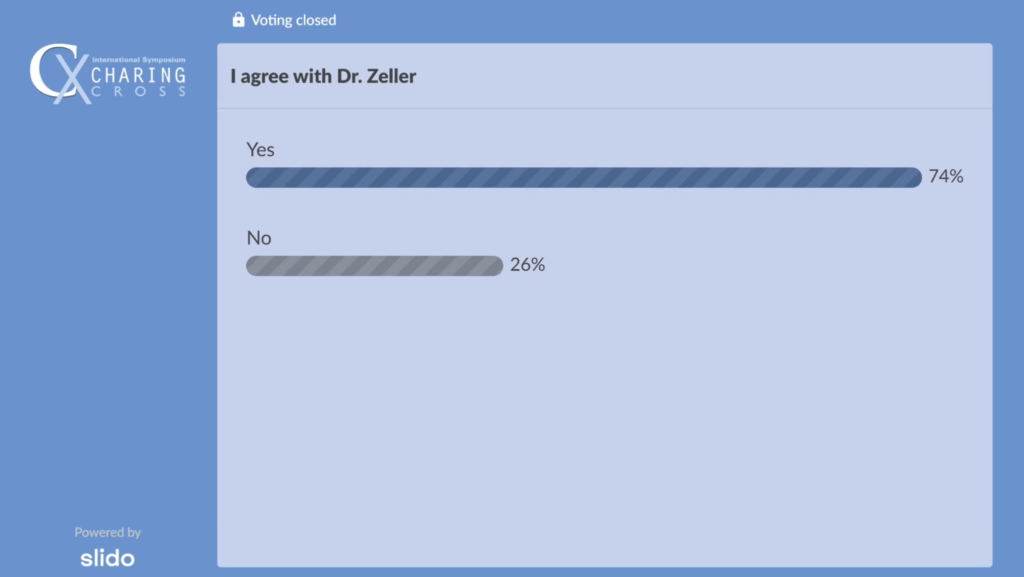
Audience polling following Zeller’s talk revealed that 74% of the audience agree it is time to change the agency recommendations regarding paclitaxel use in peripheral interventions.
“What you do not leave behind is a suboptimal result”
In a Podium 1st presentation, Gary Ansel (Columbus, USA) announced results of the IN.PACT Global stented versus non-stented analysis, comprising 353 patients stented and 1,044 non-stented patients. The purpose of this study was to compare outcomes of standalone IN.PACT Admiral DCB usage versus IN.PACT Admiral DCB followed by provisional stenting. Ansel concluded that, in this complex lesion subset from the study, the IN.PACT Admiral DCB “demonstrates durable safety and effectiveness through five years”. He added: “In the event of suboptimal angioplasty results (i.e. persistent residual stenosis >50%, flow limiting dissection), the addition of a stent did not appear to decrease the optimal results through five years”.
In the discussion following Ansel’s presentation, the presenter stressed that, regardless of whether or not you leave a stent behind, “what you do not leave behind is a suboptimal result, just to not leave a prosthetic device in. That is the worst thing to leave behind.”
Registrants can view this presentation on demand here.
Time to look at “the whole patient”
William Gray (Wynnewood, USA) delivered another Podium 1st presentation, giving the five-year results from a patient-level meta-analysis of the ILLUMENATE RCTs. He told attendees how “The Stellarex DCB continues to consistently demonstrate no difference in mortality compared to percutaneous transluminal angioplasty (PTA) year-over-year through five years, both within individual RCTs and pooled analysis.”
When asked by moderator Robert Hinchcliffe (Bristol, UK) if this was “the definitive trial to put the paclitaxel issue to bed”, Gray commented: “When you ask a US physician what puts an issue to bed, that is when the FDA rescinds their statement about danger. In order for them to do that, I think we have to see a high quality, patient-level meta-analysis that includes all the original studies included in Katsanos’ meta-analysis, followed up to five years, plus all the other datasets that have come forward since that time. The key piece here, that we do not talk enough about but we need to recognise, is that the missing data, which were on the order of 20% of the original analysis, even at the patient level, are now only about 5%, as we have gone back and done all the vital statistics. I think that will make a big difference in the ultimate analysis.”
Gary Ansel (Columbus, USA) chimed in to comment on the fact that mortality is largely due to cardiovascular issues or cancer. “I do not think we are really focussed on that,” he said. “Forget the paclitaxel, which has been really put to bed, and let us get back to good patient care and see if we can decrease those cardiovascular and cancer rates.”
Gray agreed, saying that the “major message” was that cardiovascular risk factor modifications (smoking cessation, diabetes and hypertension management) were important to consider, and that it was time to look at “the whole patient”.
Registrants can view this presentation on demand here.
All CX 2021 content is available to view on demand. Click here to access the recordings.













