Real-world outcomes from the Transcarotid Artery Revascularisation (TCAR) Surveillance Project (TSP) were presented by Mahmoud Malas from John Hopkins Hospital (Baltimore, USA) at the Society for Vascular Surgery Vascular Annual Meeting (VAM; 20–23 June, Boston, USA). At baseline, patients undergoing TCAR had significantly higher medical comorbidities before the procedure than those who were going to receive a stent, but according to Malas they were nevertheless shown in a historical dataset to experience half the risk of in-hospital transient ischaemic attacks (TIAs), stroke, and death, compared to patients undergoing transfemoral carotid artery stenting.
Although carotid stenting is a minimally invasive approach, Malas said, it has failed to have similar outcomes to endarterectomy—despite “remarkable improvement” over the last 15 years. Additionally, Malas noted, physicians are seeing almost twice as much risk of stroke with stenting, specifically in patient groups that are deemed high-risk for surgery.
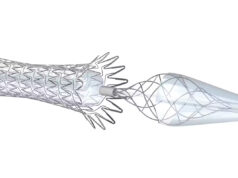
Transcarotid artery revascularisation (TCAR) is carried out by initially creating a small incision in the neck, connecting an arterial sheath to a venous sheath in the femoral vein and creating a dynamic reversal flow from high arterial pressure to low venous pressure. Malas stated that this idea was introduced as a “hybrid procedure that combines both carotid endarterectomy (CEA) and carotid artery stenting (CAS)”. By placing the clamp in the carotid artery in TCAR, the surgeon is able to provide a CEA-like protection after which a carotid stent is placed.
This technique was previously published in the Journal of Vascular Surgery and previous trials such as ROADSTER I and II (The Safety and Efficacy Study for Reverse Flow Used during Carotid Artery Stenting Procedure) have led to the approval of this technology. In relation to their outcomes, Malas pointed to the “remarkable” stroke rate of 0.7% in the ROADSTER I trial, while, at the one-year follow-up of ROADSTER II, 99% of patients were stroke free, and 95% had a stroke-free survival (n=405).
According to Malas, the ROADSTER multicentre trials reported the lowest stroke rate in high-risk patients compared to any prospective trial of transfemoral carotid artery stenting (TFCAS). However, clinical trials have selection criteria that exclude many patients, and are highly selective of operators performing procedures, which can limit the generalisability. The prospective study conducted by Malas et al therefore aimed to compare in-hospital outcomes after TCAR and TFCAS as reported by the Society for Vascular Surgery (SVS) in their Vascular Quality Initiative (VQI).
The SVS VQI TCAR Surveillance project (TSP) is intended to monitor the safety and effectiveness of TCAR in real-world outcomes. The project also aimed to compare this less-invasive surgical procedure with the standard carotid endarterectomy in centres that participate in the SVS VQI.
This prospective observational study initially intended to enrol 5,000 participants, but has just updated the dataset to 15,000 patients, with a plan to complete the study by 2024. Thus far, data from the initial 646 patients enrolled in the study were analysed and compared to patients who underwent TFCAS between 2005 and 2017.
In order to be included in the study, patients had to meet to the high-risk criteria; whether medical or anatomical. Other inclusion criteria were two or more vessels with coronary artery disease and a history of angina, congestive heart failure and/or myocardial infarction more than 72 hours and less than six weeks prior to the procedure. Patients with tandem, traumatic or dissection lesions were excluded.
The primary outcome was a composite of in-hospital mortality and neurological events (all stroke and TIAs) occurring within the patient’s hospital stay. Secondary outcomes included in-hospital mortality, ipsilateral and total stroke, transient ischaemic attacks, haemodynamic instability and hyperperfusion syndrome. Multivariate logistic regression allowed the authors to adjust for clinically significant variables and those that were significantly different between the two groups on univariate analysis.
Malas et al also carried out Coarsened Exact Matching to match patients in the TCAR group to those in the TFCAS group based on a number of variables, including usual comorbidities, degree of ipsilateral stenosis and/or the presence of anatomical or medical high-risk criteria.
Compared to patients undergoing TFCAS (n=10,136), those undergoing TCAR (n=638) were significantly older and had more cardiac comorbidities, while patients in the TFCAS group were more likely to be symptomatic and to have a restenotic lesion. There was no change in the odds of stroke or death in TFCAS over the study period (p>0.05).
Initial results
The rate of in-hospital transient ischaemic attacks and stroke, as well as composite rate of TIA, stroke and death were significantly higher in TFCAS compared to TCAR (3.3% vs. 1.9%, p=0.04 and 3.8% vs. 2.2%, p=0.04, respectively). In both procedures, symptomatic patients had higher rates of TIA, stroke, and death compared to asymptomatic patients, however the difference was significant only in the TFCAS (TCAR: 3.7% vs. 1.4%, p=0.06 and TFCAS: 5.3% vs. 2.7%, p<0.001). Furthermore, the multivariable analysis indicated that TFCAS was associated with twice the odds of in-hospital neurologic events and TIA, stroke and death compared to TCAR, independent of symptomatic status.
In relation to the limitations of the study, Malas said that so far, they have only presented outcomes in the first ~650 patients, meaning they are limited by the number. However, he reiterated that they are aiming to collect data from 5,000–15,000 patients in total. Furthermore, he touched on how they have only presented in-hospital outcomes, meaning further investigation needs to be done regarding long-term outcomes.
Nonetheless, he said, “I think this is a great example where VQI can take a new technology and evaluate it very quickly and efficiently, [especially] outside the setting of clinical trials, which are very costly and lengthy.” Malas concluded by saying that so far, they have seen very similar results in real-world outcomes for TCAR in comparison to clinical trials.
TCAR to replace endarterectomy?
Following the presentation, Malas was questioned on whether he believes it is time to switch from carotid endarterectomy to TCAR. He replied that they are “still a long way off,” with the current study needing a much larger sample. Nevertheless, he emphasised that TCAR does allow for someone who is not very experienced at carotid stenting to carry out the procedure, hence transforming the nature of it—making it easier and safer to carry out.
Discussion with the audience at VAM highlighted next steps, including a potential cost analysis comparing TCAR and endarterectomy, which Malas stated he believes to be an important issue, although no such cost analysis has yet been carried out or planned. Malas further noted that transfemoral stenting tends to end up costing more, due to the additional cost of the stent and filter. However, Malas et al also carried out a study looking at specific costs of complications. Interestingly, they found that when patients have a stroke after carotid artery endarterectomy, costs are often steeper than after carotid artery stenting, as the stroke after endarterectomy tends to be more severe. According to Malas, data within the literature supports this, revealing that strokes after carotid artery stenting are often minor.