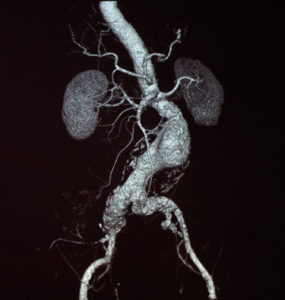
 Results of a database review of more than 500,000 abdominal aortic aneurysm (AAA) repairs revealed the majority of patients treated for rupture did not meet the criteria for aneurysm screening. These findings were reported in the August 2021 issue of the Journal of Vascular Surgery.
Results of a database review of more than 500,000 abdominal aortic aneurysm (AAA) repairs revealed the majority of patients treated for rupture did not meet the criteria for aneurysm screening. These findings were reported in the August 2021 issue of the Journal of Vascular Surgery.
According to first author Kirsten D Dansey (Beth Israel Deaconess Medical Center, Boston, USA), “Although the screening policy has likely contributed to the decrease in the incidence of ruptured AAAs, the proportion of ruptured AAAs occurring in patients currently excluded from screening is unknown. Our aim in this study was to identify the proportion of patients who had presented for AAA repair, but were not eligible for screening.”
Using the National Inpatient Sample from 2004–2015, researchers from Beth Israel Deaconess Medical Center identified ruptured and intact AAA admissions and repairs using the International Classification of Diseases codes. They evaluated 65,125 admissions for ruptured AAAs and 461,191 repairs for intact AAAs.
Current US Preventative Task Force screening criteria for AAA includes males between the ages 65 and 75 with a history of smoking. Those who did not meet the criteria for screening included:
- 68% of all patients admitted for AAAs
- 59% of patients who had undergone repair for ruptured AAAs
Of those who did not qualify for screening:
- 63% were aged >75 years
- 24% were aged <65 years
- 36% were women
Over the study period, endovascular aneurysm repair (EVAR) increased for:
- rupture from 10% to 55% with a mortality of 35%
- intact AAAs from 45% to 83% with a mortality of 2%
“The current screening guidelines are not based on modern practice data,” Dansey said. “The advantage of using EVAR is missed when calculating which patients would benefit from this low-risk procedure. Patients aged >75 years constituted more than one half of the patients admitted with AAA rupture and represent a critical and increasing screening-ineligible population. This population will realise an especially high benefit of undergoing repair on intact AAAs, given the difference in mortality of 45% after repair of rupture AAAs vs 1.3% after repair of intact AAAs.”
The authors noted that the UK’s National Institute for Health and Care Excellence (NICE) guidelines for AAA diagnosis and management found benefit for AAA screening for a prevalence as low as 0.35%.
According to Dansey, “It would be reasonable to conclude that screening women, who have a prevalence of AAA of 1.7% (reported for women with a positive smoking history) would be cost-effective, as was recommended in the NICE guidelines.”
Dansey further stated, “The number of ruptured AAA admissions has decreased over time, suggesting that screening and implementation of EVAR have had a positive effect. However, the number of repairs for rupture AAAs has remained unchanged, suggesting that screening remains underutilised.”
Researchers concluded most patients who had undergone repair for ruptured AAAs did not qualify for screening and EVAR was the primary treatment of both ruptured and intact AAAs with relatively low in-hospital mortality. Based on their findings, the team suggested that expansion of the screening criteria to include selected women and a wider age range should be considered.













