Gerard Stansby, Newcastle, UK, told delegates at CX35 (6–9 April 2013, London, UK) that the use of glue in varicose veins in safe and effective and that, if it continues to show good results, it will be a very attractive procedure for the future.
Stansby noted that cyanoacrylate glue, also called superglue, has been around for a long time, with a wide range of applications both biologically and in other aspects of daily life. Presenting background information for the material, Stansby said that the original cyanoacrylates were discovered in 1942 in a search for materials to make clear plastic gun sights during World War II.
“Cyanoacrylates are the main liquid adhesives used for endovascular procedures. It has been used for gastrointestinal bleeding embolisation, direct endoscopic injection and embolisation of vascular malformations, including intracranial embolisations. We know a lot about the substance, and I think it is fair to conclude that it is safe and effective. There have been some problems with glue emboli, but this was very rare,” Stansby stated. He added that “cyanoacrylate can cause some tissue toxicity locally, but in a way that is how they work, by inciting an acute inflammatory response. Sarcomas in rodents have been described with a particular type of cyanoacrylate but no malignancies have ever been reported in humans”.
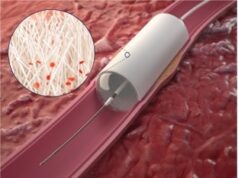
The VenaSeal Sapheon closure system (Sapheon) is a commercially developed system for applying superglue in varicose veins. Stansby explained that the catheter is advanced up to close to the saphenous femoral junction and the ultrasound transducer is used to produces some compression down on the end of the catheter, where the glue will be released. The glue is released in small blobs sequentially down from the saphenous femoral junction from a puncture lower down on the leg.
He showed ultrasound images of the catheter in place and also a duplex colour image showing how the colour flow stops in the section of the vein that has been treated with the glue. He also showed histological images demonstrating how the vein is occluded through an inflammatory and fibrotic process with cellular ingrowth.
“One of the advantages of this technique is that you do not need to use any compression stockings after the treatment,” he said. “Other advantages of using glue are that it is very easy to do as an ambulatory procedure, treating the whole long saphenous vein from one puncture; because there is no heat involved, there is no need for any tumescent anaesthesia and no risk of thermal damage to nerves or skin.”
A pilot study with eight patients receiving small volumes (1.58ml) of glue has been conducted. Subsequently, 38 patients were followed for one year, with no significant side effects or complications. Stansby noted that in the initial group there was a significant number (21%) who had thrombus extension through the saphenous femoral junction, although there were no clinical problems. He said that the technique has been modified since then and now it is recommended that the first injection is done 5cm below the saphenous femoral junction. “It is a bit lower than most of people must be used to do with radiofrequency and other techniques,” he said.
Recently, the “European multicentre study on cyanoacrylate embolisation of refluxing great saphenous veins without tumescent anesthesia and without compression therapy” by Proebstle et al was published in abstract form in the Journal of Vascular Surgery: Venous and Lymphatic Disorders. It followed 69 patients treated with a median follow-up of three months. It reported complete occlusion rates of 95% at three months and 90% occlusion rates at six months. No serious adverse events were observed. There were six cases (8.7%) of phlebitis and one patient had 0.5mm thrombus extension into the common femoral vein.
Stansby told delegates: “Cyanoacrylate glue is a CE-marked product. lt is perfectly appropriate to use on your patients, but I think we need more long-term data. The company is starting a randomised controlled trial, and that will be very helpful, but I think longer-term cohort follow-up is also needed.”
He added, “Glue is clinically attractive, because it is particular suitability for ambulatory use with no tumescence anaesthesia required. At the moment, at least in the UK, it is a quite expensive technique, which means it is difficult to pursue in the National Health Service (NHS). It has not gone through the NICE approval process for the NHS yet. If it continues to show such good results, however, it will be a very attractive procedure for the future.”