José L Soriano (University of Granada, Granada, Spain) and colleagues propose a strategy for the wound healing of burns in Pharmaceutics that combines the antioxidants vitamins A, D, E with the endogenous pineal hormone melatonin (MLT), all loaded into a thermosensitive hydrogel delivery system.
They report that the formulation showed “optimal antimicrobial activity”, comparable to a commercial reference, and that it exhibited “the strongest healing process” in the skin burns of rats when compared to hydrogel-alone, MLT-loaded hydrogel, vitamin-loaded hydrogel, and an assayed commercial reference containing silver sulfadiazine. This led Soriano et al to conclude that “The use of an antioxidant cocktail of vitamins and MLT might be a promising treatment for skin wounds for future clinical studies”.
The investigators set out to assess the skin wound healing efficacy of this “antioxidant cocktail”, following previous work from the same group that separately evaluated the effect of vitamins A, D, E and MLT formulated in hydrogel of poloaxamer 407 (PLX), chitosan (CS), and hyaluronic acid (HA) aimed for skin wound healing. This earlier studies evidenced “great” healing properties on induced skin burns, the authors say, while being biocompatible with healthy skin.
In the present study, Soriano and colleagues conducted a variety of tests to determine any skin wound healing properties of their formulation. The antioxidant efficacy and microbiological activity against Gram positive and Gram negative strains were assayed using the Kirby-Bauer disk diffusion susceptibility test. Use of the blank hydrogel, without the additions of the vitamins or MLT, showed no radical scavenging activity (RSA), the authors report. Statistically significant differences from the blank hydrogel were observed when MLT-alone and vitamins-alone were used, with RSA values of ~18% and ~52%, respectively. The values of RSA for the full antioxidant cocktail—vitamins A, D, and E with MLT, loaded into the hydrogel (PLX/CS/HA-VM)—were significantly higher, in the vicinity of 70%.
Concerning microbiological activity, Soriano et al write: “It is clear that PLX/CS/HA and PLX/CS/HA-VM produced significant inhibition of bacterial growth; they were roughly similar to the commercial reference, except in the case of E. coli ATCC 25922, for which both the blank hydrogel and the loaded hydrogel did not show antimicrobial action. Similar results were obtained in the case of growth inhibition assay.”
Elaborating on these positive results, the investigators clarify: “Despite these results, this antimicrobial action cannot be considered as an antibiotic agent, but it demonstrated huge potential to efficiently prevent the wound from bacterial infection and, thus, might provide a synergistic effect, acting like a disinfectant to the wound healing action of vitamins.”
In vivo testing supports skin healing efficacy of the vitamin-MLT-loaded hydrogel formulation
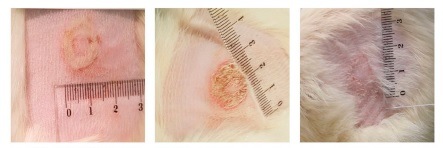
Skin healing efficacy was tested using an in vivo model and a histological evaluation. The research team conducted their in vivo wound healing study in rats: the animals were shaved, cleaned with 70% ethanol, and then divided into groups of three individuals. Skin burns were caused by a 1cm2 superficial contact area of cylindrical devices at 100°C. The treatments were then applied once daily for two weeks in different ways for each group. Group I was the positive control; the rats in this group received no treatment. In group II, the animals were treated with 100µL of PLX/CS/HA without antioxidant actives. Group III rats were treated with 100µL of PLX/CS/HA-VM (VM denoting vitamins A, D, and E, and MLT). In the fourth group, the animals were treated with the commercial reference silvederma (a silver sulfadiazine cream from Cathay Drug).
The results of this skin healing efficacy test were positive for the study authors’ formulation. They detail their findings: “Wounds treated with PLX/CS/HA-VM exhibited similar healing progress to those treated with the commercial reference silvederma. After 14 days, a significant acceleration in wound healing was observed as compared with animals treated with the unloaded PLX/CS/HA hydrogel and the untreated group.”
Wound closure was recorded by the measurement of the wound size and applying the following equation: wound healing (%) = (initial wound size minus final wound size) divided by (initial wound size) X 100. This was 54.23% in the untreated group, 63.52% in animals treated with the blank hydrogel, 96.12% for the group treated with PLX/CS/HA-VM, and 98.53% for the group treated with the commercial reference.
Soriano et al also performed a histological analysis on the excised burned areas of skin to further assess the wound healing capabilities of their formulation. They quantified the neutrophil number per 5µm sample, counting in three random foci of the dermis and using a light microscope for visualisation.
“In the case of untreated animals,” they write, “an ulcer and the presence of inflammatory cells covered by a scab could be observed. The tissue also showed increased epidermal thickness and a loss of epidermal appendices such as hair follicles. A similar pattern was observed in skin samples treated with blank hydrogel, although the scabs were smaller. In specimens treated with the commercial reference silvederma, epidermis growth showing wound contraction could be observed. The groups treated with vitamin-loaded hydrogel and MLT-loaded hydrogel also showed a good recovery, similar to the commercial reference group. However, it seems that in conjunction they could ameliorate the regeneration of the epidermis and dermis, as it can be observed from the histological evaluation of samples treated with PLX/CS/HA-VM, in which both groups of antioxidant actives were included. In this last case, skin showed less infiltration of inflammatory cells, smaller epidermal thickness, and more epidermal appendices when compared to the commercial reference treatment.”













