Endovascular aneurysm repair with the Fenestrated Anaconda stent graft (Vascutek) delivers “satisfactory short-term technical and clinical success rates in patients with juxtarenal, suprarenal, and type IV thoracoabdominal aortic aneurysms,” according to new research published in the Journal of Endovascular Therapy. The authors of the study report that mid-term aneurysm sac regression and target vessel patency “appear very good”.
Drosos Kotelis, RWTH Aachen University Hospital, Aachen, Germany, and colleagues write that, with the introduction of fenestrated stent grafts, the general move from open towards endovascular aneurysm repair has now reached the juxta- and suprarenal levels of the abdominal aorta.
Although controlled trials comparing endovascular aneurysm repair (EVAR) with open repair are still lacking, Kotelis at al note that most retrospective analyses of the published data demonstrate noninferiority of the endovascular approach regarding perioperative mortality and morbidity in anatomically suitable patients.
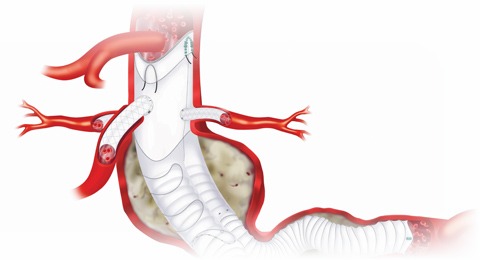
Fenestrated EVAR, unlike open surgery, requires specific anatomic criteria that need to be met for the patient to be suitable for the procedure. “For example, the suprarenal and infrarenal aortic neck angulations should not be too great, the target vessels should not be in close proximity, and both iliac axes should be patent for target vessel cannulation,” the authors explain. The fenestrated Anaconda device was introduced in 2010 to broaden some of these anatomic criteria. “The initial experience with this new endograft was promising, but overall published outcomes are very limited,” Kotelis and colleagues write. “The largest published series of 25 patients with an 11-month median follow- up reported 4% operative mortality and 96% target vessel patency. However, data are lacking about the performance of the device in the longer term.”
The research team conducted a single-centre retrospective analysis of 39 consecutive patients (median age 74 years; 36 men) treated with the Fenestrated Anaconda stent graft between July 2011 and December 2015. Indications for fenestrated EVAR were abdominal aortic aneurysms with neck anatomy unsuitable for a standard stent graft. Median infrarenal neck length was 4mm (range 0–9mm). Four (10%) patients presented with type IV thoracoabdominal aortic aneurysm, 12 (31%) with suprarenal aneurysms, and 23 (59%) with juxtarenal aneurysms. Four (10%) patients had previous infrarenal aortic repair. Five (13%) patients had an infrarenal neck angulation >60 degrees. A total of 106 fenestrations were incorporated into the stent grafts (73 renal arteries, 25 superior mesenteric arteries, and eight celiac trunks). Technical success, perioperative and mid-term mortality and morbidity, target vessel patency, endoleaks, and reinterventions were documented.
Technical success was achieved in 95% (37/39) of patients. Three (8%) patients died in-hospital; two from mesenteric embolism and one from renal artery rupture with consequent multiorgan failure. Two (5%) patients suffered an intraoperative embolic stroke. During a median follow-up of 33 months (range 4–55 months), adjunctive manoeuvres were performed in nine (23%) patients, including reintervention for type II endoleak with enlarged aneurysm sac in two (5%) cases. Four additional patients died of causes unrelated to the aortic pathology; overall mortality was 18%. In 34 (94%) of the 36 patients seen in follow-up, aneurysm sac size was stable or had decreased, while target vessel stent patency was 99% (95/96).
“The overall 99% rate of target vessel patency after a median follow-up of almost three years demonstrates the midterm durability of these endovascular reconstructions,” explain the authors. They continue, “The high rate (94%) of aneurysm sac shrinkage/stabilisation and the absence of an aneurysm-related death during follow-up also reflect the efficacy of fenestrated EVAR in this group of patients. Finally, since the majority of reinterventions were required in the first year after fenestrated EVAR, we, like other groups, would also advocate a more individualised surveillance protocol in these patients, aimed at reducing the number of computed tomographic angiographies by substituting duplex ultrasound in patients with documentation of sac shrinkage and patent target vessels.”












