In an official Society response, SVS president Joseph Mills tackles recent coverage in the mainstream media of inappropriateness in vascular care.
There have been several recently published articles by respected news media outlets highlighting the deeply concerning issue of the overuse of invasive procedures to treat peripheral arterial disease (PAD). The front-page New York Times article (Sunday, July 16, 2023), first-authored by Katie Thomas, serves as the exclamation point. The Society for Vascular Surgery (SVS) appreciates the efforts of the NYT to call attention to the inappropriate use of interventions in an effort to raise patient awareness, promote quality and advocate for safety in the delivery of vascular care.
The SVS has more than a 75-year history of setting the standards of care, quality and safety for patients with PAD. Founded in 1946, and comprising more than 6,000 members, the SVS mission is to advance excellence in vascular healthcare through education, advocacy, research and public awareness. Our mission and code of ethics focus on doing what is best and most appropriate for the care of patients with vascular disease, despite the challenges created by a struggling healthcare delivery system and problematic regulatory/reimbursement policies. We are troubled to see reports of patient harm because of the violation of the fundamental ethos of all physicians and surgeons to “first do no harm.” However, we are also concerned that such articles will cause patients to mistrust the healthcare system and delay seeking appropriate and timely care for limb- and sometimes life-threatening PAD.
It is essential for the public, affected patients and their family members, to understand there is only one primary specialty in medicine comprehensively educated, trained and tested to provide the full spectrum of evidence-based care to vascular patients, ranging from medical management to minimally invasive procedures, to open surgery. That specialty is vascular surgery. The vast majority of SVS members are vascular surgeons, board-certified by the Vascular Surgery Board (VSB) of the American Board of Surgery (ABS), who practice daily with integrity and are dedicated to appropriate and ethical care. Unfortunately, there are outliers practicing far beyond the pale who stretch ethical boundaries and deviate from the best available science and evidence-base. Within the NYT article, regarding the procedure highlighted, it was noted that “from 2017–2021, about half of Medicare’s atherectomy payments—$1.4 billion—have gone to 200 high-volume providers.” It should be noted that none of the physicians detailed in this NYT story is a board-certified vascular surgeon or SVS member. As the article also documents, after failed attempts at limb salvage by other practitioners, patients end up in the vascular surgeon’s care only as a last resort, sometimes far too late to save a precious limb.
The overwhelming majority of vascular surgeons, and a vast majority of other specialists that receive some training and play a role in the care of vascular patients, including those trained in vascular medicine, interventional cardiology, and interventional radiology, are providing high-quality, evidence-based care with safety and the best patient outcomes in mind. Appropriate and safe vascular care can be delivered in both outpatient and hospital settings.
Unfortunately, as in all professions and trades (albeit more disturbing in the healthcare arena), there are outliers who overstep the bounds of ethics, appropriateness and quality, perhaps driven by other motivations, including notoriety or financial gain. This is a complex issue that requires the examination not only of the events detailed in this story, in which several patient experiences with the physicians that provided their care were highlighted, but of the underlying healthcare economic, legal and regulatory policies that created fertile soil for this behavior to germinate and take root.
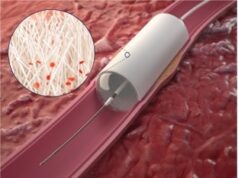
The issue of overuse in medical care is not a new one. Scientific, peer-reviewed articles written by SVS members and vascular surgeons were among the first to call attention to potential patient harm resulting from the aggressive overuse of interventions for patients with PAD largely brought about by regulatory and reimbursement coverage decisions that financially incentivized such therapy. These studies documented a dramatic increase in atherectomy procedures primarily performed in an outpatient setting with extremely high-volume users (outliers) more likely to be non-vascular surgeons treating patients early after a diagnosis of claudication. As one example of a highly reimbursed procedure of unproven value, roughly 50% of Medicare reimbursements for atherectomy went to just 200 high-volume providers.
The article also alludes to the potential for the development of improper relationships between industry and healthcare practitioners as one factor that may drive inappropriate use or overuse of drugs and devices for financial gain. A detailed discussion of this issue is not possible here, but there is no doubt that the medical industry of drug and device manufacturers is essential to the provision of healthcare and innovation in therapy. Many widely available and highly useful drugs and devices (stents, endovascular grafts, etc.) have been developed by ethical, scientific collaboration between practicing physicians and surgeons and the healthcare technology industry. As do most other medical societies, the SVS has a policy on conflict of interest and conflicts of commitment.
These ethical principles underpin and guide all we do, not only as a medical organization, but also as individual practitioners. The needs of the patient should always come first; no procedure should be recommended or performed in any patient if it is not primarily and solely for the benefit and best interests of that patient.
The SVS has been the leading national organization in defining quality and safety standards for the provision of comprehensive vascular care, particularly for PAD. There are an estimated 10–12 million people in the U.S. who have PAD, so it is important to educate patients and the public about PAD and how it should be treated. The disease is caused by the build-up of plaque deposits in the walls of arteries due to a combination of risk factors, including diabetes, smoking, hypertension, hyperlipidemia, increased age and genetics. PAD is a broad spectrum of disease; in general, it is a marker for cardiovascular disease and the most common complication to develop in affected patients is not limb loss, but rather heart attacks and stroke. Thus, all patients with PAD should have best medical therapy and control of their risk factors to the extent possible. There are three stages of PAD: asymptomatic, claudication (leg cramping or pain with walking) and chronic limb-threatening ischemia (CLTI=non-healing wound or gangrene).
Only the latter has a significant risk of limb loss, and even in CLTI patients, the risk depends upon the stage of disease. Through the publication of research studies, evidence-based guidelines and appropriate use criteria documents, the SVS has consistently promulgated the principle that the best care for the majority of patients with PAD—particularly those who are asymptomatic—is to promote exercise (walking) and to manage the PAD medically by modifying correctable risk factors such as elevated lipids, diabetes, smoking and hypertension.
PAD is common, particularly in older people, but not all leg pain is directly related to PAD—even in those who have the disease. For example, arthritis, gout, musculoskeletal and spinal problems can all cause leg and foot pain. Even for patients who have pain with walking from PAD, the majority are best treated initially with risk-factor control, walking therapy to promote collaterals, and muscle adaptation to exercise and occasionally medicines specific for vascular leg pain brought on by walking (since fewer than 5% of patients with claudication progress to a limb-threatening PAD stage). Vascular surgeons are uniquely trained and positioned to understand the full context and spectrum of PAD and all of the available treatment options. As such, it has been the position of the SVS that a first intervention for PAD patients—even a “minimally invasive procedure”—should be done only when absolutely necessary, as once completed, it may “accelerate the clock” and speed the progression of vascular disease and its complications.
Invasive procedures for claudication may improve function and quality of life but patients should be selected carefully, and the interventions tailored to be both safe and likely to produce meaningful benefit. The SVS practice guidelines have proposed a threshold of at least two years of likely durability for an intervention performed for claudication. There is a disturbing trend of overly aggressive treatment, with recent studies demonstrating nearly 30% of patients are receiving interventions on below-the-knee arteries, despite no evidence they would benefit and mounting evidence it may accelerate their disease. Moreover, the article highlights the growing frequency of multiple, repeated procedures that is emblematic of poor patient selection and inadequate durability of the chosen procedure, leading to a vicious cycle of repetitive interventions that is not only costly, but also dangerous.
There are patients with PAD (perhaps 5–8%) who suffer from or progress to the most advanced PAD stage, that of CLTI. This condition is more prevalent in people with diabetes. Preventing amputation in such patients hinges upon early and accurate diagnosis, followed by an individualized treatment plan targeted to the patient’s risk, goals and stage of disease. Such a plan is best carried out with the involvement of a vascular surgeon, and frequently includes other specialists, such as podiatrists. The SVS spearheaded and published classification systems to assess risk of limb loss, an anatomic staging system and global guidelines for evidence-based care to save limbs and prevent amputations. Although many CLTI patients require intervention, endovascular therapy is only one option, and a good number of patients fare better with surgical bypass. Vascular surgeons are the only specialists trained to offer both options, when needed. Patients deserve to be fully informed when making decisions about invasive treatments.
Vascular surgeons have also pioneered tracking patient outcomes. To this end, the SVS established its Patient Safety Organization (PSO) to monitor outcomes of patient care, which now includes 1,007 participating centers, and has collected the outcomes of more than 1 million vascular interventions within its Vascular Quality Initiative (VQI) registries. In addition, in collaboration with the American College of Surgeons, the SVS recently launched it Vascular Verification Program, setting standards of quality across vascular care settings. Vascular surgeons are actively engaged in and leading the effort to promote shared decision-making and patient education around PAD care, including the message that while an abnormal ankle brachial index (ABI)—a noninvasive measure of blood flow to the leg/foot—or the symptom of claudication can be important warning signs, the best therapeutic response is most often best medical therapy, not the “quick fix” of an intervention performed unnecessarily or prematurely.
As reported in another recent article by ProPublica, SVS feels strongly that the public at large and the vascular patient population should be educated and have access to all the resources they need to make the best choices for their care, including being provided with an explanation of the natural history of their condition, the expected outcomes of medical and interventional therapy, and understanding the differences between a variety of types of providers who perform some vascular procedures compared to board-certified vascular surgeons who provide the full spectrum of vascular care.
The SVS will continue to actively promote quality and safety for vascular patient care through its published guidelines, appropriate care documents, PSO-VQI registry and initiatives such as the Vascular Verification Program. All practitioners in vascular practice are encouraged to become familiar with and to utilize them. The SVS will continue to develop these resources and make them available.
The SVS encourages patients to check and verify the credentials of their providers before agreeing to a plan of vascular care. We also encourage second opinions. Finally, in their efforts to cover health news, the SVS urges media professionals to be diligent in presenting healthcare and medical information that is fully balanced, as coverage could lead to patient distrust and delays in necessary care with potentially adverse consequences.
Joseph Mills is president of the SVS. He was writing on behalf of the SVS Executive Board.