Findings from a first-of-its-kind study conducted at University Hospitals (UH) Harrington Heart & Vascular Institute (Cleveland, USA) showed a novel system-wide interdisciplinary team assembled to evaluate alternative treatments to major amputation improved outcomes for patients with chronic limb-threatening ischaemia (CLTI). The findings were recently published in Circulation: Cardiovascular Interventions from the American Heart Association.
Clinical decisions approving amputation are frequently made in isolation by a patient’s individual caregivers, a UH press release states. To address this problem, UH Harrington Heart & Vascular Institute created a novel system-wide interdisciplinary team called the Limb Salvage Advisory Council (LSAC) and evaluated its impact on a specific population of patients who were already scheduled for amputation. According to UH, only one quarter (excluding those who died or were lost to follow-up) of the patients formerly scheduled for a major amputation actually lost a limb at 180 days after being managed by LSAC.
“Circulation issues often cause painful cramping, numbness and wounds which can greatly decrease a person’s quality of life. When a doctor suggests amputation to address the pain, patients usually follow that recommendation, yet nearly half of all people with vascular disease will die within five years of an amputation. This is higher than the five-year mortality rates for breast cancer, colon cancer and prostate cancer,” said Mehdi Shishehbor, president of UH Harrington Heart & Vascular Institute, and Angela and James Hambrick chair in Innovation.
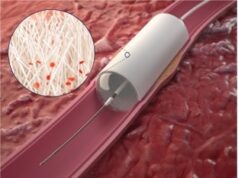
Shishehbor leads UH’s limb salvage programme, which uses minimally invasive approaches to restore blood flow to dying limbs and prevent amputation.
The LSAC at UH includes vascular surgeons, endovascular interventionalists, vascular medicine specialists, podiatrists, and wound care experts. Once a patient who is scheduled for a major amputation is identified, the treating physician may elect to notify a designated coordinator who arranges for an urgent virtual LSAC meeting. LSAC members review and discuss available data including comorbidities, functional status, extent of tissue loss, relevant imaging studies and prior interventions with the goal of providing diversified thoughtful inputs. Eventually, the LSAC reaches one of two conclusions: the limb is salvageable and a plan is created to save it, or the patient is approved to proceed with the originally scheduled amputation.
The press release details that, statistically, amputees are disproportionately of lower socioeconomic status, and that African Americans are up to four times more likely to have an amputation than white Americans.
“UH is committed to improving the health of all people by advancing science and human health. All people should have the opportunity to receive the necessary medical resources and support to have a healthier life, regardless of their status in the community or their race,” said Shishehbor. “We believe that broad implementation of this policy nationwide could really help people and significantly reduce amputation rates across the USA.”
A total of 19 patients who were scheduled for major amputation underwent LSAC evaluation between January and September 2019. The patients had a mean age of 63. Three patients were deemed unsalvageable due to extensive tissue loss and proceeded with their originally scheduled amputation, while the other 16 patients were considered for limb salvage. Fifteen patients had successful revascularisation. Nine of them had not undergone major amputation at 180 days and six of them had complete healing or significant reduction in wound size in that time.
UH claims that this is the first study investigating the impact of a novel and proactive interdisciplinary intervention on patients already planned for a major amputation due to CLTI. Two studies have reported on the adoption of multidisciplinary care in CLTI and improved outcomes; however, both were retrospective and had revascularisation proceduralists from a single specialty.
“Our interdisciplinary LSAC is unique because it involves not just multiple teams including endovascular interventionalists and vascular surgeons, but often multiple physicians within the same specialty. This ensures different points of view and more potential options to avoid amputation,” said Tarek Hammad, interventional cardiologist at UH Harrington Heart & Vascular Institute. “It is important to foster a culture of mutual respect and trust within the team and among various specialties to avoid judgement and competition.”
These findings may have significant policy implications if all patients scheduled for major amputation were mandated to receive an evaluation with an interdisciplinary team such as LSAC, UH asserts, adding that widespread implementation of this policy could greatly reduce scheduled amputations. This cause could be further helped by future research exploring how to move the referral to LSAC further upstream allowing for early intervention, the press release concludes.