Midterm results from a study of the largest population of patients with no-option chronic limb-threatening ischaemia (CLTI) treated with percutaneous deep vein arterialisation (pDVA) using the LimFlow device show that, in this complex group of patients, this treatment method is feasible, with a high technical success rate and amputation-free survival at six through to 24 months, coupled with effective wound healing. In selected patients with no-option CLTI, percutaneous deep vein arterialisation could be a recommended treatment to prevent amputation and heal wounds, Costantino Del Giudice (Université de Paris, Paris, France) told delegates attending the online 2020 meeting of the Cardiovascular and Radiological Society of Europe (CIRSE; 12–15 September, virtual).
These results from the ALPS (midterm outcomes of percutaneous deep venous arterialization with a dedicated system for patients with no-option chronic limb-threatening ischemia) multicentre study were published in the Journal of Endovascular Therapy in May this year, and appeared in the August print issue, in addition to being presented at the CIRSE congress. The ALPS registry is the largest study to date of no-option CLTI patients treated with the LimFlow system reporting mid- and long-term results, and is a multicentre, retrospective study conducted at centres in Alkmaar, The Netherlands; Leipzig, Germany; Paris, France; and Singapore encompassing 32 end-stage—or “no-option”—CLTI patients.
The investigators set out to evaluate the midterm results of patients suffering from no-option CLTI treated with a dedicated system (the Limflow system) for percutaneous deep venous arterialisation. Thirty-two consecutive CLTI patients (mean age 67±14 years; 20 men) were treated with this method using the Limflow device at four centres between 11 July 2014 and 11 June 2018 and retrospectively analysed. Of all patients, 21 (66%) had diabetes, eight (25%) were on immunosuppression, four (16%) had dialysis-dependent renal failure, nine (28%) had Rutherford category six ischaemia, and 25 (78%) were deemed at high risk of amputation. The primary outcome was amputation-free survival (AFS) at six months. Secondary outcomes were wound healing, limb salvage, and survival at six, 12, and 24 months.
Technical success was achieved in 31 patients (96.9%). The median follow-up was 34 months (range 16-63). At six, 12, and 24 months, estimates were 83.9%, 71%, and 67.2% for AFS, 86.8%, 79.8%, and 79.8% for limb salvage, and 36.6%, 68.2%, and 72.7% for complete wound healing, respectively. Median time to complete wound healing was 4.9 months (range 0.5–15). The deep vein arterialisation circuit occluded during follow-up in 21 patients; the median time to occlusion was 2.6 months. Reintervention for occlusion was performed in 17 patients: 16 because of unhealed wounds and one for a newly developed ulcer.
Deep vein arterialisation a hope for “no option” patients
“No option” patients are those where no possible endovascular or surgical procedure will help, due to either the absence of a target vessel or thanks to unsuccessful prior interventions. These patients frequently have calcified vessels, diabetes mellitus, dialysis, and/or long-term corticoid therapy. The risk of amputation and persistent wound is 58% when these patients are treated with conservative therapy, and the risk of death at one-year follow-up is 20%.
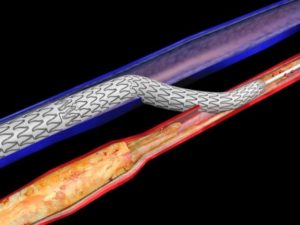
Deep vein arterialisation aims to improve the blood flow to the foot. “We direct nutritional improvement by reversal of flow through venules,” Del Giudice told the CIRSE audience, describing how deep vein arterialisation works. “This stimulates arteriogenesis, and recruits hibernating collaterals.”
The most important step, he shared, is patient selection. “Patients have to have a good heart function, a good life expectancy, foot arteries not treatable by an endovascular or surgical approach, a Rutherford class 5–6, a Wound, Ischaemia, and Foot Infection (Wifi) score of 3, and no infection,” Del Giudice listed.
According to the speaker, the Limflow technique is the most commonly used method.
The Limflow technique: How it works
Del Giudice talked CIRSE registrants through a case demonstrating the use of the Limflow technique. This first involved performing arteriography and venography scans to aid target vessel selection. Next, the interventionalists advanced the venous and arterial catheters to the target vessel, where the artery and vein were closest, and created an arteriovenous fistula, bridging the two vessels. Then, they advanced the guidewire along the vessel, using it to push the balloon through the arteriovenous fistula to create a passage. Blood flow is diverted from the blocked artery into the vein to salvage the lower leg.
Del Giudice also shared an alternative technique whereby entry in the distal lateral or medial plantar vein from a subintimal channel in the plantar artery can be intentionally pursued as a bailout tactic; this involves pointing the tip of the guidewire opposite to the arterial wall calcifications.
Yet another method is the venous arterialisation simplified technique (VAST). This utilises a low-profile balloon catheter and a snare to facilitate arteriovenous fistula creation during venous arterialisation.
An arteriovenous fistula could also be created using a low-profile balloon catheter and an outback catheter. Del Giudice described a case where he and his team treated a patient using this method, explaining how the patient had occlusion of the popliteal artery. “Without any target vessel in the distal leg,” he said, “we performed subintimal ligation towards the posterior tibial artery, and then we used the outback [catheter] to advance the balloon into the posterior tibial vein, and create the [arteriovenous] fistula, advancing the guidewire. Finally, we performed a valvotomy with a low-profile balloon, and stented the vein from the ankle to the arteriovenous fistula.”
Showing a table comparing the outcomes at six months from these different techniques, Del Giudice was positive: “There is good primary patency, ranging from 40–90% at six months, and good wound healing outcomes, ranging from 40–100%. Major amputations ranged from 0–33.3% at six months follow-up.”
Earlier trials: The Promise I study
PROMISE I study was an early feasibility study launched in mid-2017 to establish the clinical safety of the Limflow technique. It aimed to provide enough data for the investigators to move on to a pivotal trial, to identify and address any operator challenges, and to determine patient characteristics and therapeutic parameters that impact performance. Enrollment was completed in 2019, and the triallists have since reported a 97% technical success rate in the 32 patients treated in the USA as part of this study. Overall survival was 96%, freedom from amputation was 77%, and amputation-free survival was 74%.
“The importance of this study was that it allowed us to understand that not all patients are candidates for this procedure. We need salvageable tissue to obtain some results,” Del Giudice told the CIRSE audience. “Moreover,” he continued, “the results [show that] this is quite different from an arterial canalisation. Deep vein arterialisation requires four to six weeks for tissue granulation to start. Oedema can occur in the treated limb after deep vein arterialisation, but typically resolves within three to four weeks. We need to preserve native arterial perfusion and mange pedal loop outflow during the maturation process. It is also important to monitor changes in foot tissue colour. In terms of wound care, multidisciplinary collaboration is required, and patients may need some minor amputation management, debridement.”













