Barry T Katzen, founder and medical director of Baptist Cardiac & Vascular Institute (BCVI), Miami, USA, is considered one of the founders of interventional radiology as a medical specialty and is one of the few non-surgeons awarded membership in the Society for Vascular Surgery in the United States. He spoke to Vascular News about the founding of BCVI and the occasion when he treated leg aneurysms in US vice president, Dick Cheney. Katzen also spoke about the evolution of interventional radiology, the use of live cases for educational purposes, his involvement with the SAPPHIRE trial and his current areas of research.
When did you decide you wanted a career in medicine? Why interventional radiology?
I wanted to be a physician for as long as I can remember, probably around the age of eight. As a child I was very involved in working around the animal labs at the hospital, and got involved in science projects at school, winning some American Heart Association awards. As far as interventional radiology is concerned, it did not exist when I started my career. It has been an honour to be considered one of the pioneers of this discipline, and it reflected well my interests in clinical medicine and reluctance about leaving it for a radiology residency. It was those early formative years that shaped the direction of my career towards innovation and clinical patient care.
Who has inspired you in your career and what advice of theirs do you remember today?
I had the traditional ‘angiographic’ training of the time, and was actually the chief of section of CV Radiology at St Vincent’s hospital when I went to Rome, in 1974, to study with Plinio Rossi at the University of Rome; all at the request of my hiring institution, where he had been for 13 years prior. While only three months in duration, it was a transformational experience for me and everyone who was there at that time. In fact, when I returned to New York, my colleagues could not believe I was the same person. Professionally and technically, what we shared was an incredible personal chemistry, learning the spirit of innovation, ‘respect for tissue’ and the rush of the challenge of changing the status quo. Friendships for life were made and still exist today.
What have your proudest moments been?
From a professional viewpoint, this is a very difficult question. I think the founding and subsequent building of the first multidisciplinary integrated care facility, in what now is BCVI, has been one of the top ones. And now, as we are on the threshold of a major new expansion and extension of our original vision, I know this will be an enduring entity. Perhaps more importantly, I am extremely proud of the interventional radiology and vascular surgeon’s team we have built. Among the interventional radiology partners, each of them could be a section or department chief anywhere, and they continue to be part of our collaborative effort and team.
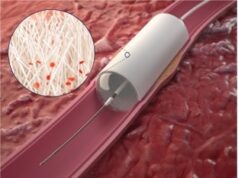
As with any interventionalists, the first of anything is always a moment of pride, and some of them include, starting an angioplasty programme in New York (the first since Dotter) prior to balloon catheters, first percutaneous transluminal renal angioplasty, TIPS, 5th endograft in the USA. Of course, being asked to lead the team treating the sitting vice president of the United States, Dick Cheney, in 2005, was one of my all time career highlights. The fact that we had to perform, under fairly high pressure circumstances, an unapproved procedure with an unapproved device, and doing both lower extremities during the same session was perhaps one of my most memorable cases, and may still today be the only bilateral popliteal aneurysm case done simultaneously. I still have my White House M&M candies!
Finally, one of my most passionate efforts has been to transform interventional radiology into a clinical discipline. This is what I have practiced by example throughout my career, what we have made a living and breathing model at BCVI and what is gradually beginning to occur throughout interventional radiology, at least in the United States.
How has interventional radiology evolved since you began your career?
We started this discipline without knowing what direction we were going in. It was clear, that through using imaging we could effect change in the human body less invasively but we did not have tools. Every case was a first for something as we explored the potential benefits of less invasive therapies. As it became clear, we had a movement and possibly a specialty on our hands and there was a lot of discussion about what we should call it. Many called for endosurgery, ie endovascular surgery, endobiliary surgery, endourology, etc. At that time, the political environment would have tolerated those terminologies and perhaps would have been better. The biggest changes that have occurred surrounded the regulatory changes which have transformed the ability for individual doctors to ‘explore’ better solutions for patients, in the USA at least. At BCVI we still do, but it is more and more challenging. Also, interventional radiology has had to learn how to collaborate in a multidisciplinary world, since we have created and continue to create procedures that other disciplines will adopt.
Which technique or technology had a profound effect on your career?
In my early years, during the time when vascular surgery opposed percutaneous transluminal angioplasty, it was certainly angioplasty and lysis. In the early years, I developed a wire (Katzen wire) that is still sold today (I believe 20+ years later). I saw the great potential for improving patient care, and the urgent need to train qualified physicians rather than waiting for the traditional residency time period. This is why I initiated a video education in 1978 at Alexandria Hospital, Virginia, USA. This became the symbolic procedure of interventional radiology, although we were making major advances in all aspects of image guided therapies like: gastrointestinal bleeding treated with catheter directed drugs and embolisation and relief of obstructed biliary and genitourinary systems with drainage catheters. However, it was only in the vascular space where surgeons were opposing advancement. Of course there were a few who did not, and on a personal level, I have always had strong support from my vascular surgery colleagues, and anyone looking for the best outcomes for their patients.
At every stage of my career there has been a key vascular surgeon who I partnered with: Jesse Blumenthal in New York, Alan Deutsch in Alexandria, and Jack Yaffa, Steven Kanter, Jose Alvarez, and Orlando Puente in Miami, among others. In those early years, these colleagues were frequently ostracised by their surgical colleagues. I will always appreciate their support.
Having been involved in the SAPPHIRE trial, how do you analyse the results of CREST?
The CREST data represent a landmark for carotid artery stenting. While I am writing this, the FDA has granted Abbott the low risk labelling they have been requesting. We have come a long way from SAPPHIRE, but still have a long way to go. Carotid artery stenting is a procedure that should be performed by the highest qualified interventionalists, regardless of discipline, but with measurable and accountable outcomes. I think, in five years, it will be a much more important part of the treatment armamentarium. I still believe the trial against best medical therapy should be conducted, and that most patients with asymptomatic disease should be managed medically.
The International Symposium on Endovascular Therapy (ISET) has been running for 23 years. What makes ISET so popular?
The programme directors of ISET continue to bring innovation to medical education. It is very challenging in today’s environment to maintain the value proposition necessary to attract registrants. This is our primary goal – to be the provider of unique and high quality educational content, which the registrant can use in the next week, and to bring the community together to consider the future of our field, in a multidisciplinary way.
You support the use of live cases for education purposes. How can these be made safe?
To us, the use of live case education provides the most valuable method of educating practitioners about procedures they are doing. These things cannot be taught as well in books, or other media sources. Live case education will always reflect real world therapy, and of course, it becomes a statement on the quality of work and value structure of the team and institution involved.
We maximise patient safety in a number of ways. This include: extensive discussion and review by the whole team in advance of the programme; working with multiple physicians at one time to reduce the multitasking pressures created by live case education; complete informed consent and post ISET debriefings on our own performance. I still most enjoy teaching by the bedside and whether this is on a routine basis with whoever is in the room or to a large group, my performance and approach is the same. It remains a critical method of expanding the role of endovascular therapy. But, being a great physician does not make you a great teacher, and being a great teacher does not make you a great live case operator and teacher. Like everything else, it takes a combination of knowledge, talent, ability to multitask, and comfort with modern media.
The Baptist Cardiac & Vascular Institute developed a multidisciplinary approach back in the 80s. How has it contributed to the success of the institution?
The multidisciplinary culture created in the 80s cannot be overestimated in terms of its value. It has allowed us to be more competitive in the marketplace locally, achieve incredible levels of measurable quality, patient, employee and physician satisfaction, and most importantly prepared us long in advance for increasing the integration required to move forward the field of endovascular therapy for procedures such as complex aortic and structural heart procedures. While this is not something we promote externally, we frequently get comments from patients that everyone is working together for their benefit. From the beginning of the institute we have felt that turf battles were destructive and that collaboration was constructive. This palpable result has led to capital commitment by the institution, and most recently a commitment of US$60 million to expand BCVI and broaden our mission and programmes.
How do you see the endovascular field developing in the future?
Our field will continue to expand as we develop more less invasive and better solutions for vascular disease and continue to increase patient awareness. We are at the threshold of great advances in the imaging environments and the potential to improve the image-guided part of what we do is very important. Our procedures will get less and less invasive and hopefully they will not be devalued as a result.
What are your current areas of research?
Important areas for us include: defining the role of drug elution for peripheral arterial disease, exploring the role of intervention in hypertension and other diseases that we may be able to alter the physiology as well as the anatomy, understanding whether endovascular therapy really has a role in multiple sclerosis, and stroke prevention through medical therapy and interventional techniques. Cell therapy may also become an important part of our approaches to critical limb ischaemia.
Outside of medicine, what are your interests?
I really enjoy boating of any type and have a powerboat. I enjoy fishing with my buddies (non doctors) on the weekends, when we get a chance. In the past, my wife and I have done a lot of cruising on our own boat (Wandering Star was the name), but my time on the water is a little differen. It is the way I get ‘down time’ from the usual pace I am running at. My current boat is called Down Time too. My career has allowed us to travel as well. I also love spending time (not enough) with my two grandchildren. And of course, none of this could have happened without the support of my loving wife Judi. We have been married for 44 years and have known each other since high school.
Fact File
Training
1966–1970 Medical School, University of Miami School of Medicine, Miami (early admission)
1970–1971 Internship, Jackson Memorial Hospital, Miami, Florida (Straight Medicine)
1971–1974 Radiology Residency, The New York Hospital – Cornell Medical Center, USA
1974–1975 Fellowship, St Vincents Hospital/Medical Center, Cardiovascular Radiology, New York
Foreign studies
Sep–Nov 1974 Angiography, Policlinico Umberto Primo, Instituto di Radiologia “La Sapienza”, University of Rome, Italy (Plinio Rossi, director)
Sep–Oct 1973 Pulmonary Radiology and Chest Special Procedures, The Brompton Chest Hospital, London, UK (Ian Kerr, director)
Jun–Aug 1969 Chest Pathology, National Institute of Health Grant, The Brompton Chest Hospital (Lynne Reid, director)
Current appointments
Jul 1987–present Medical director/founder, Baptist Cardiac & Vascular Institute, Baptist Hospital of Miami
Jul 1987–present Voluntary professor of radiology, University of Miami School of Medicine, Miami
Jul 2005–present Assistant professor of radiology, University of South Florida, Tampa, USA
Jan 2000–present Courtesy professor, Biomedical Engineering Institute, Florida International University
2010–present Associate dean for clinical affairs for Baptist Health, FIU Herbert Wertheim College of Medicine
2010–present Clinical professor of radiology, FIU Herbert Wertheim College of Medicine
2010–present Clinical professor, Department of Surgery, voluntary, FIU Herbert Wertheim College of Medicine
Professional societies
American College of Angiology, American College of Cardiology, Fellow American College of Gastroenterology, Fellow American College of Radiology, Fellow American Heart Association, Fellow American Medical Association, American Roentgen Ray Society, Cardiovascular and Interventional Radiological Society of Europe, Member Chesapeake Vascular Society, DC Chapter of Radiology, International Society for Cardiovascular Surgery, New York Roentgen Society, Radiological Society of North America, Fellow Society of Interventional Radiology, Southeastern Angiographic Society Virginia, Medical Society Florida Vascular Society, South Florida Vascular Society, Society for Vascular Surgery.
Awards and recognitions
Listed in Best Doctors in America (1982); Gold Medal Recipient, University of Miami Alumni Association (1997); Best Doctors in America (1998); Diagnostic Imaging Magazine: Radiology’s 20 Most Influential (1998, 2002); Gold Medal Recipient Society for Cardiovascular and Interventional Radiology SIR (2002); member of medical team responsible for repairing vice president Dick Cheney’s popliteal aneurysm (2005); Gold Medal Recipient, Cardiovascular and Interventional Radiological Society of Europe CIRSE (2006); Cordis: Leaders In EndoVascular Education Award (2006); Iron Arrow, University of Miami, U of M’s highest honour (2007); American Heart Association Council on Cardiovascular Radiology and Intervention Distinguished Achievement Award (2008); American Heart Association Awarded the 2010 Cor Vitae Heart Award (2010);America’s Top Doctors 2002; America’s Top Doctors (2007); Best Doctors of America (2007/2008); Florida Super Doctors – South Florida Edition (2008); Best Doctors of America (2009)